Proximal Humerus
- Diagnosis
- Non-operative Options
- Operative Options
- Before Your Surgery
- After Your Surgery
- Your Rehab
The humerus is the upper arm bone and it forms two joints —shoulder joint and elbow joint. The proximal humerus is the upper end of the arm bone that forms the shoulder joint. Fractures of the proximal humerus are common in elderly individuals suffering from osteoporosis.
Causes of Proximal Humerus Fractures
Proximal humerus fractures are caused by traumatic injuries such as a fall on an outstretched hand from a height or motor vehicle accidents. In younger individuals, a severe trauma can cause these fractures.
Types of Proximal Humerus Fractures
Proximal humerus fractures can be categorized into 4 groups:
- Greater Tuberosity Fractures: Greater tuberosity is the insertion site for attachment of rotator cuff tendons. Greater tuberosity fractures are less common and are seen in cases of shoulder dislocations and in those with osteoporosis. Greater tuberosity fragment is pulled off when the cuff muscle contracts or the anterior shoulder dislocates. Direct impact to the shoulder causes the tuberosity bone to break into multiple fragments. Partial rotator cuff tears often accompany non-displaced fractures and these fractures can be diagnosed using MRI or diagnostic arthroscopy.
- Lesser Tuberosity Fractures: These fractures are often caused by posterior shoulder dislocations or traumatic muscle contractions by electrical shock or convulsions. If left untreated, these fractures cause subscapularis muscle (stabilizer and mobilizer muscle) deficiency and require a major muscle transfer procedure.
- Surgical Neck Fractures: Fractures of the surgical neck are most common in patients with osteoporotic bone. These fractures also damage the axillary nerve that carries sensory information from the shoulder.
- Humeral Head Fractures: Humeral head fractures very often occur in elderly individuals and chances are more in those with osteoporotic bone. These fractures occur in younger individuals by significant trauma, whereas a mild traumatic injury can cause fracture in elderly individuals with osteoporosis.
In addition to the above, other types of proximal humerus fractures are two, three, and four-part fractures. A fracture causes multiple fragmentation of the proximal humerus.
Symptoms of Proximal Humerus Fractures
Patients with proximal humerus fracture experience severe pain, swelling, and restricted motion of the shoulder.
Diagnosis of Proximal Humerus Fractures
Proximal humerus fracture is diagnosed by a physical examination, X-ray of the affected area and/or computerized tomography (CT) scan.
Want to know more?
Most proximal humerus fractures are minimally displaced and can be treated with conservative approaches such as use of a sling to immobilize and early physical therapy to improve the functional outcome.
Want to know more?
Surgery may be necessary in displaced fractures. The multiple fragments are fixed with plates, screws or pins and in severe cases shoulder replacement surgery is performed.
Want to know more?

Once you and your doctor decide that surgery will help you, you will need to learn what to expect from the surgery and how to actively participate in the treatment plan for the best results afterward.
Preparing mentally and physically for surgery is an important step toward a successful result. Understanding the process, and your role in it, will help you recover more quickly and have fewer problems.
Before surgery, your doctor will perform a complete physical examination to make sure you don’t have any conditions that could interfere with the surgery or the outcomes.
- Routine tests, such as blood tests and X-rays may be performed.
- Discuss any medications you are taking with your doctor as you may have to stop or alter your intake before surgery. If you are taking aspirin or anti-inflammatory medications or any drugs that increase the risk of bleeding, you will need to stop taking them one week before surgery to minimize bleeding.
- Discuss with your doctor about preparing for potential blood replacement, medical interventions and other treatments prior to surgery.
- Report any infections to your surgeon. Surgery cannot be performed until all infections have cleared up.
- If you smoke, you should stop or cut down as smoking interferes with wound healing and can affect your recovery.
- Have someone available to take you home, as driving is not recommended for at least 24 hours or as advised.
- You may need help with everyday tasks such as cooking, shopping and laundry.
- Put items that you use often within easy reach, so you won’t have to stretch and bend as often.
- After Surgery Video
- Shoulder Surgery Recovery Video
Want to know more?
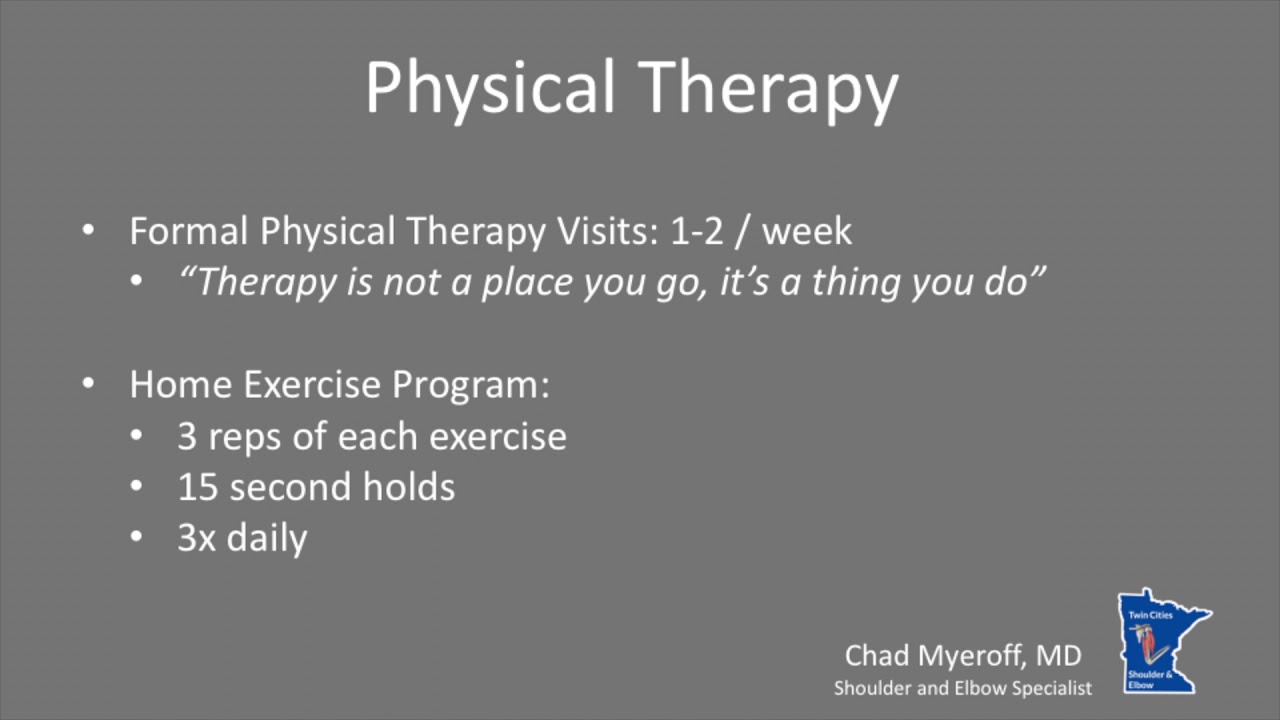
- Physical Therapy Intro Video
- Finger ROM Video
- Standard Elbow ROM Video
- Shoulder ROM Video
Following surgery there is a minimum period of immobilization after which rehabilitation should begin. As early as the first post-operative day, you will be made to move your arm as much as you can without too much pain. Physical therapy starts with passive/assisted range of motion exercises. Activities of daily living can slowly be introduced but there must be no lifting or shoulder movements against resistance for at least 6 weeks. Strengthening and stretching should then begin gradually with resistance exercises. It is necessary to monitor progress in movement and strength as persistent weakness may indicate a rotator cuff tear or nerve damage.