Shoulder Arthritis
- Diagnosis
- Non-operative Options
- Operative Options
- Before Your Surgery
- After Your Surgery
- Your Rehab
The term arthritis literally means inflammation of a joint but is generally used to describe any condition in which there is damage to the cartilage. Damage of the cartilage in the shoulder joint causes shoulder arthritis. Inflammation is the body's natural response to injury. The warning signs that inflammation presents are redness, swelling, heat and pain.
The cartilage is a padding that absorbs stress. The proportion of cartilage damage and synovial inflammation varies with the type and stage of arthritis. Usually the pain early on is due to inflammation. In the later stages, when the cartilage is worn away, most of the pain comes from the mechanical friction of raw bones rubbing on each other.
What are the Types of Shoulder Arthritis?
There are over 100 different types of rheumatic diseases. The most common are osteoarthritis and rheumatoid arthritis.
Osteoarthritis
Osteoarthritis is also called as degenerative joint disease; this is the most common type of arthritis, which occurs often in older people. This disease affects cartilage, the tissue that cushions and protects the ends of bones in a joint. With osteoarthritis, the cartilage starts to wear away over time. In extreme cases, the cartilage can completely wear away, leaving nothing to protect the bones in a joint, causing bone-on-bone contact. Bones may also bulge, or stick out at the end of a joint, called bone spurs.
Osteoarthritis causes joint pain and can limit a person's normal range of motion (the ability to freely move and bend a joint). When severe, the shoulder joint may lose all movement, making a person disabled.
Rheumatoid Arthritis
This is an auto-immune disease in which the body's immune system (the body's way of fighting infection) attacks healthy joints, tissues and organs. Occurring most often in women of child-bearing age (15-44), this disease inflames the lining (or synovium) of joints. It can cause pain, stiffness, swelling, and loss of function in joints. When severe, rheumatoid arthritis can deform, or change a joint.
Rheumatoid arthritis affects mostly joints of the hands and feet and tends to be symmetrical. This means the disease affects the same joints on both sides of the body (both hands or both feet) at the same time and with the same symptoms. No other form of arthritis is symmetrical. About two to three times as many women as men have this disease.
Causes of Shoulder Arthritis
Osteoarthritis is caused by the wearing out of the cartilage covering the bone ends in a joint. This may be due to excessive strain over prolonged periods of time, or due to other joint diseases, injury or deformity. Primary osteoarthritis is commonly associated with ageing and general degeneration of joints.
Secondary osteoarthritis is generally the consequence of another disease or condition, such as repeated trauma or surgery to the affected joint, or abnormal joint structures from birth.
Rheumatoid arthritis is often caused when the genes responsible for the disease is triggered by infection or any environmental factors. With this trigger, the body produces antibodies, the defense mechanism of the body, against the joint and may cause rheumatoid arthritis.
Symptoms of Shoulder Arthritis
There are several forms of arthritis and the symptoms vary according to the form of arthritis. Each form affects the body differently. Arthritic symptoms generally include swelling and pain or tenderness in the joints for more than two weeks, redness or heat in a joint, limitation of motion of a joint and early morning stiffness.
In an arthritic shoulder:
- The cartilage lining is thinner than normal or completely absent. The degree of cartilage damage and inflammation varies with the type and stage of arthritis.
- The capsule of the arthritic shoulder is swollen.
- The joint space is narrowed and irregular in outline; this can be seen in an X-ray image.
- Bone spurs or excessive bone can also build up around the edges of the joint.
Diagnosis of Shoulder Arthritis
Doctors diagnose arthritis with a medical history, a physical exam and X-rays of the affected part. Computed tomography (CT) scans and magnetic resonance imaging (MRI) scans are also performed to diagnose arthritis.
Want to know more?
- Shoulder Joint Replacement
- Reverse Total Shoulder Replacement
- Physical Therapy Intro
- Shoulder and Elbow Steroid Injection
There is no cure for arthritis, so beware of 'miracle cures'. Your doctor may prescribe anti-inflammatory medicine. He/she may recommend occupational therapy or physiotherapy, which includes exercises and heat treatment.
Want to know more?
In severe cases, surgery may be suggested. The type of surgery will depend on your age and severity of the condition. In the elderly with severe arthritis, joint replacement can give good results. Common surgery for treatment of shoulder arthritis is arthroplasty (replacement of the damaged joint). It may be total shoulder arthroplasty or hemiarthroplasty.

Once you and your doctor decide that surgery will help you, you will need to learn what to expect from the surgery and how to actively participate in the treatment plan for the best results afterward.
Preparing mentally and physically for surgery is an important step toward a successful result. Understanding the process, and your role in it, will help you recover more quickly and have fewer problems.
Before surgery, your doctor will perform a complete physical examination to make sure you don’t have any conditions that could interfere with the surgery or the outcomes.
- Routine tests, such as blood tests and X-rays may be performed.
- Discuss any medications you are taking with your doctor as you may have to stop or alter your intake before surgery. If you are taking aspirin or anti-inflammatory medications or any drugs that increase the risk of bleeding, you will need to stop taking them one week before surgery to minimize bleeding.
- Discuss with your doctor about preparing for potential blood replacement, medical interventions and other treatments prior to surgery.
- Report any infections to your surgeon. Surgery cannot be performed until all infections have cleared up.
- If you smoke, you should stop or cut down as smoking interferes with wound healing and can affect your recovery.
- Have someone available to take you home, as driving is not recommended for at least 24 hours or as advised.
- You may need help with everyday tasks such as cooking, shopping and laundry.
- Put items that you use often within easy reach, so you won’t have to stretch and bend as often.
- After Surgery Video
- Shoulder Surgery Recovery Video
- Post-operative Sling
After the surgery, pain medications and antibiotics are prescribed to control pain and prevent infection. Your arm may be secured in a sling or cast.
Want to know more?
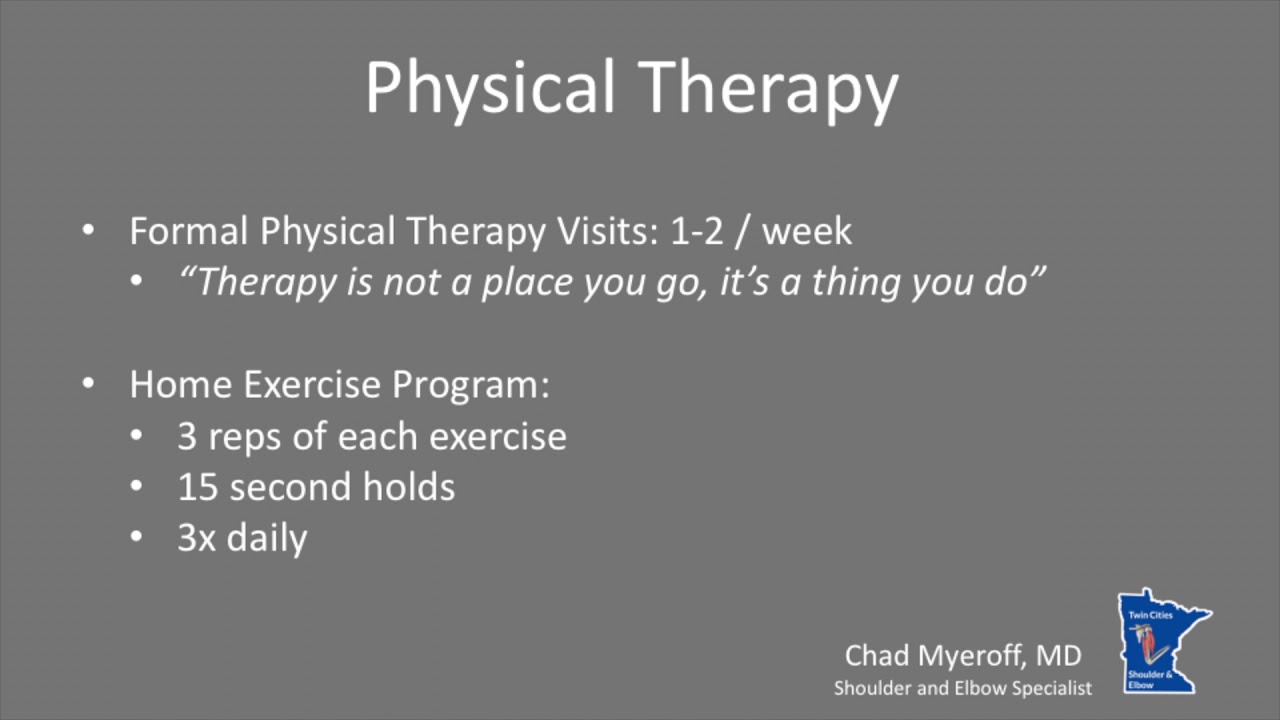
- Physical Therapy Intro Video
- Finger ROM Video
- Standard Elbow ROM Video
- Shoulder ROM Video
The rehabilitation program includes physical therapy, which is started soon after the surgery and is very important to strengthen and provide mobility to the shoulder. You may be able to perform gentle daily activities two to six weeks after surgery.
Want to know more?
- Download Dr. Myeroff's Shoulder Stretches Information Sheet
- Download Dr. Myeroff's Standard Elbow ROM Diagram Information Sheet
- Download Dr. Myeroff's Finger ROM Diagram Information Sheet
- Download Dr Myeroff's Post-Op Protocol for Anatomic Total Shoulder Arthroplasty / Hemiarthroplasty
- Download Dr Myeroff's Rehab Protocol for Reverse Total Shoulder Arthroplasty