Distal Radius Fractures
- Diagnosis
- Non-operative Options
- Operative Options
- Before Your Surgery
- After Your Surgery
- Your Rehab
The forearm consists of two bones, the radius and ulna. The radius is the larger of the two forearm bones, and the region towards the wrist is called the distal end. Fractures in this end are most common.
The distal radius can be broken in various ways, but generally occurs around 1 inch from the distal end of the wrist. The most commonly occurring distal radius fracture is the Colles fracture, which leads to an upward tilting of the broken radius bone. Other types of distal radius fractures include:
- Intra-articular fracture: Fracture extending into the wrist joint
- Extra-articular fracture: Fracture not extending into the wrist joint
- Open fracture: Fractured bone, which breaks through the skin
- Comminuted fracture: Bone fractured into more than two pieces
Causes
Falling onto an outstretched arm is the most common way to fracture the distal radius. Other causes include:
- Minor falls with the presence of osteoporosis (fragile bones)
- Major trauma to the wrist during a vehicular accident
Symptoms
The symptoms occurring with distal radius fractures include bruising, swelling, immediate pain and tenderness, and limited mobility. The broken wrist may also appear deformed.
Diagnosis
Your doctor will diagnose distal radius fractures by ordering an X-ray of the wrist to detect broken or displaced bone. Your doctor can also view the number of pieces the bone is broken into from the X-ray images. Sometimes, a computer tomography (CT) scan may be required to get a detailed view of the fractured fragments.
You can protect your wrist with a splint and apply an ice pack while keeping the wrist elevated until the doctor examines it. The choice of treatment will depend on your age, level of activity, nature of fracture and your surgeon’s preference.
If the bone is aligned properly even after the fracture, a plaster cast may be enough to allow it to heal on its own. In case the broken bones are misaligned, realignment of the broken fragments may be required. For this, your doctor may perform closed reduction, which involves moving the broken bone pieces into place and straightening the bone without opening the skin. After alignment of bones, your doctor will place a splint or cast on your arm. The splint may be used initially for a few days till the swelling subsides, after which a cast may be added. The cast may be changed after a few weeks as it loosens with the reduction in swelling.
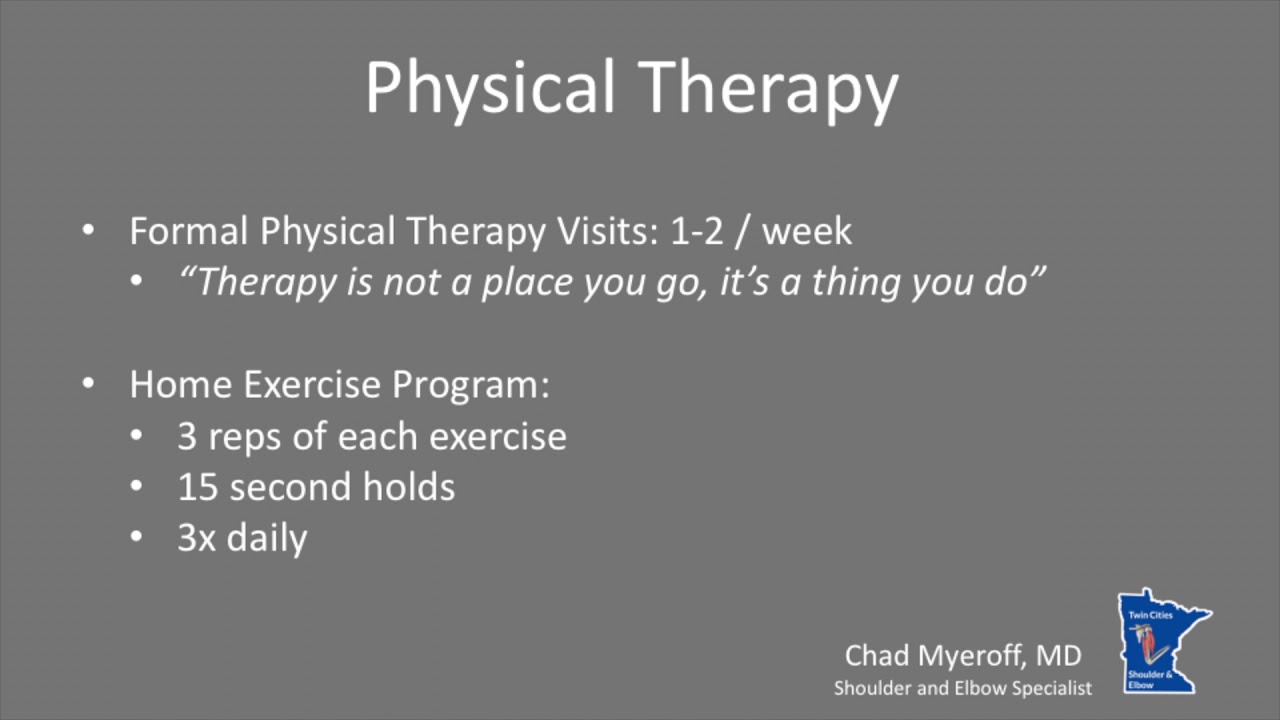
The healing process will be monitored with regular X-rays. After the cast is removed, the doctor may recommend physical therapy to help improve the function and motion of your injured wrist.
Surgical therapy is recommended for fractures that are completely displaced and cannot be corrected with a cast. Open reduction technique involves directly accessing and aligning of the broken bones through an incision. After alignment, the bones can be secured together in the correct position with the use of any of the following or a combination of these techniques:
- Cast
- Plate and screws
- Metal pins (titanium or stainless steel)
- External fixation (outside the skin stabilising frame to hold the bones in its aligned position until it heals)
Open fractures: Surgery is recommended for all open fractures within a few hours after the wrist injury. The bone and exposed soft tissues are thoroughly cleaned, antibiotics are administered to prevent infections, and internal fixation methods are used to hold the broken bones in correct position. For badly damaged soft tissues, a temporary external fixator may be placed. The internal fixation screws or plates may be placed after several days in a separate procedure.

Once you and your doctor decide that surgery will help you, you will need to learn what to expect from the surgery and how to actively participate in the treatment plan for the best results afterward.
Preparing mentally and physically for surgery is an important step toward a successful result. Understanding the process, and your role in it, will help you recover more quickly and have fewer problems.
Before surgery, your doctor will perform a complete physical examination to make sure you don’t have any conditions that could interfere with the surgery or the outcomes.
- Routine tests, such as blood tests and X-rays may be performed.
- Discuss any medications you are taking with your doctor as you may have to stop or alter your intake before surgery. If you are taking aspirin or anti-inflammatory medications or any drugs that increase the risk of bleeding, you will need to stop taking them one week before surgery to minimize bleeding.
- Discuss with your doctor about preparing for potential blood replacement, medical interventions and other treatments prior to surgery.
- Report any infections to your surgeon. Surgery cannot be performed until all infections have cleared up.
- If you smoke, you should stop or cut down as smoking interferes with wound healing and can affect your recovery.
- Have someone available to take you home, as driving is not recommended for at least 24 hours or as advised.
- You may need help with everyday tasks such as cooking, shopping and laundry.
- Put items that you use often within easy reach, so you won’t have to stretch and bend as often.
- After Surgery Video
- Elbow Surgery Recovery Video
- Elbow Elevation Technique Video
Want to know more?
- Physical Therapy Intro Video
- Finger ROM Video
- Standard Elbow ROM Video
Want to know more?
- Download Dr. Myeroff's Elbow Elevation Technique Information Sheet
- Download Dr. Myeroff's Standard Elbow ROM Diagram Information Sheet
- Download Dr. Myeroff's Finger ROM Diagram Information Sheet
- Download Dr Myeroff's Post-Op Protocol for Distal Radius Fracture – Non-op
- Download Dr Myeroff's Post-Op Protocol for Distal Radius Fracture – ORIF